What is Infantile Hemangioma?

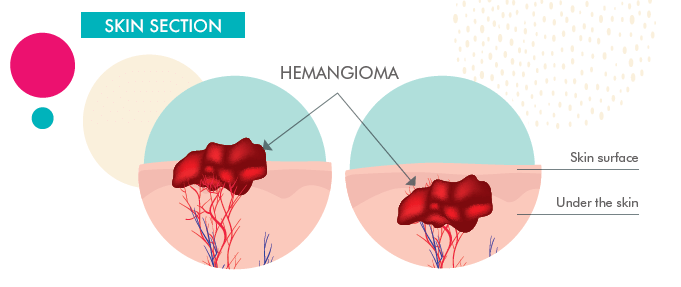
Hemangiomas can appear anywhere on the body but are most common on the face or neck. They can be flat like a birthmark, form a nodule, or have a plaque-like texture and appearance.
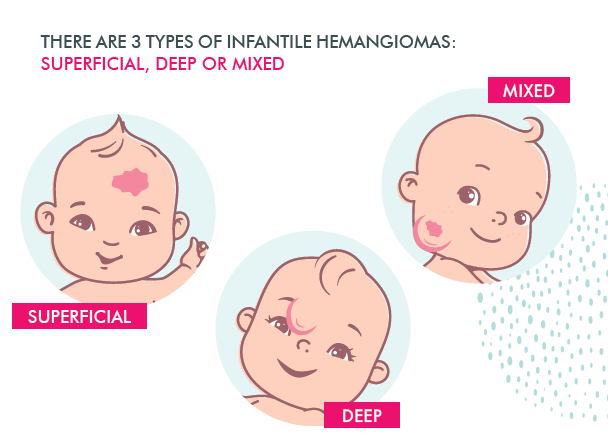
Superficial Hemangiomas
Superficial hemangiomas occur on the surface of the skin and are flat and reddish in color. This is normally what people think of when they picture infantile hemangiomas.
Deep Hemangiomas
Deep hemangiomas form below the surface of the skin. They tend to have a bluish appearance.
Compound Hemangiomas
Compound hemangiomas have both the traits of superficial and deep hemangiomas.
After determining that your baby has an infantile hemangioma, talk to your baby’s doctor right away. Diagnosing your baby with the right type of hemangioma is crucial for proper treatment.
Why Does My Baby Have Infantile Hemangioma?
At this point, medical science doesn’t fully understand what causes infantile hemangiomas. It is known that babies with certain traits have a higher risk of developing IH. This includes infants born with low birth weights, females, Caucasians, and premature babies.
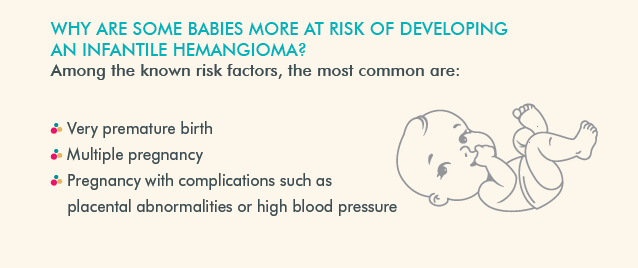
The most important thing to remember is that if your baby has an IH, that is not a sign that you did anything wrong as a parent. Since their cause is unknown and the condition is relatively common, it’s unknown how to prevent them. IHs are not the result of parental negligence (and are often harmless). Keep in mind that your baby’s infantile hemangioma is not your fault.
Also keep in mind that accurate diagnosis and early treatment, if necessary, is key. If your baby has an infantile hemangioma, focus on what you can control, which is making sure your baby’s hemangioma is being properly addressed and treated.
Is Infantile Hemangioma Contagious?
Infantile hemangiomas are not a sign of communicable disease, which means they aren’t contagious. Rest assured that your baby can engage in all the normal activities other children can, including crawling, playing, eating, sleeping, and exploring the world around them. All your family members can still safely hug and hold your baby.
Is Infantile Hemangioma a Serious Condition?
Infantile hemangioma is normally not a serious condition. Most IHs are small, purely cosmetic, and may even disappear over time on their own without any treatment.
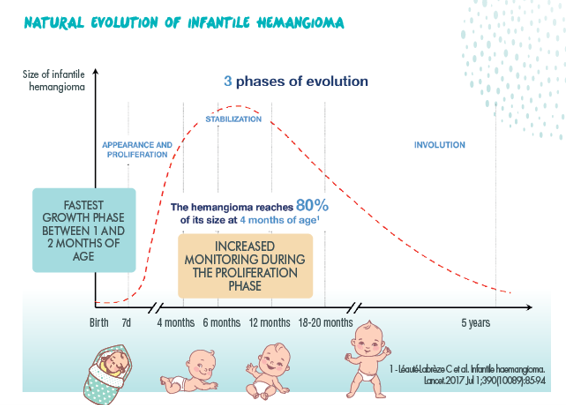
Infantile hemangiomas usually show up soon after birth and tend to grow quickly. Most infantile hemangiomas will be 80% fully formed at 3 months after birth. Expect any hemangiomas to reach their full size at about 5 months.
Early identification and intervention are key (ideally before your baby is 1 month old), especially if your baby’s hemangioma has the potential to be problematic down the road. So even though your baby’s hemangioma is most likely harmless, it always pays off to mention it to your doctor just to make sure.
Infantile Hemangioma Potential Complications
In severe cases, IH can interfere with your baby’s healthy development (5,6). If your baby’s hemangioma developed on their eyes, it can affect their vision, especially since eye development is crucial while your baby is young. Hemangiomas on the nose can at times affect breathing by blocking airways. And hemangiomas on the mouth can impact your baby’s ability to eat and swallow food.
In these cases, IHs require intervention and treatment so your baby can grow up happy and healthy.
Visceral Hemangiomas
Sometimes, hemangiomas grow internally. These are known as visceral hemangiomas. Visceral hemangiomas can be very dangerous and tend to be harder to detect. Because of their severity, they often need immediate medical intervention. They tend to occur in the liver, intestines, airway, and brain. Jaundice can be a sign of liver hemangiomas, while blood in the stool can be a sign of intestinal hemangiomas. If your baby has a croupy cough or difficult breathing, talk to their doctor – that can be a sign of hemangiomas blocking the airway.
Babies that have multiple hemangiomas (a condition called hemangiomatosis) are at higher risk of developing visceral hemangiomas. Because of this, babies with hemangiomatosis should be checked for internal lesions. If your infant has more than 3 hemangiomas, their doctor may order an ultrasound of the entire body to check for internal lesions.
Hemangiomas as Indicators of Other Concerns
At times, IHs can also be a sign of an underlying issue. Intracranial or aortic arch vascular abnormalities are often accompanied by large facial hemangiomas. Because of this overlap, it’s especially important to talk to your baby’s doctor if their hemangioma is on their face or head.
Risk of Bleeding
Some IHs are susceptible to bleeding. Over time, if left untreated this can lead to anemia, infection, and/or needing blood transfusions. Like any other wound, bleeding hemangiomas can also be very painful for your baby, so they shouldn’t be left unaddressed.
Skin Changes
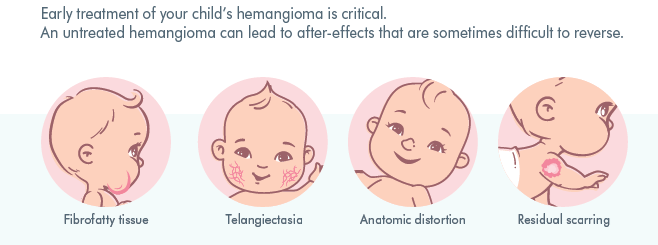
Although most IHs resolve on their own by the time children reach 7 to 9 years, they often leave behind permanent skin changes. About 69% of hemangiomas can leave permanent residual lesions if untreated. This can include scars, extra skin, extra fatty tissue, and the like. And about 1 in 3 facial hemangiomas will result in disfigurement from permanent soft tissue distortion.
While these are often cosmetic, they can still be problematic for the child, especially if they’re in a spot that isn’t generally covered by clothing. Because of the potential for permanent skin changes, there’s a window of opportunity to address an IH.
Why Should You Consult a Physician?
As soon as a lesion appears, do not hesitate to consult a physician, who will keep an eye on the hemangioma.
In the vast majority of cases, infantile hemangioma do not present any complications and disappear on their own.
90% of hemangiomas are small, non-problematic, and can be easily covered by most clothing. These will not require medical attention or intervention. However, 10% of children with hemangiomas will need to be examined by a specialist and may need to consider further treatment. This can either be for cosmetic reasons or because the hemangioma may impact proper functioning.
When should you consult a Physician?
Only about 30% of hemangiomas are visible at birth. Most hemangiomas don’t appear until the first few weeks, or sometimes even months, after birth. And they tend to grow after their first appearance. IHs grow fastest between 1 and 3 months of age.
If you notice this happening, don’t panic. Check your baby often, taking note of any new or changing marks on their body. Just as you probably count your baby’s ten fingers and ten toes, keep an eye on any distinctive markings and mention them to your baby’s doctor right away – particularly if they’re changing or growing. Even though most IHs are harmless, identifying and diagnosing them early on is key
As soon as an infantile hemangioma appears, It Is vital to consult your baby’s doctor. Increased monitoring during the proliferation phase is important. The doctor will arrange for regular follow-up visits or refer your child to a doctor with expertise in infantile hemangioma.
Do not hesitate to report any changes in the size or appearance of the infantile hemangioma to your doctor. The earlier it is treated, the more likely it is to disappear quickly and without any after-effects.
It may be helpful to take pictures of your child’s hemangioma regularly so that your doctor can more easily monitor its progress.
How is the diagnosis made?
The diagnosis and determination of the degree of severity of the infantile hemangioma are made during the clinical examination.
Your doctor or the pediatric hemangioma expert will assess the severity of the hemangioma by considering:
- Your child’s age
- The number and location of the hemangioma(s)
- The size of the hemangioma and its appearance (color, thickness, ect)
- Its evolution: is the hemangioma growing or stable? Photos of your child since birth can be of great help.
In some cases, the doctor may need to perform additional tests (medical ultrasound MRI scan, ect) to confirm the diagnosis.
Treatment for Infantile Hemangioma
Hemangeol, a beta-blocker, is the first and only FDA-approved treatment for infantile hemangiomas requiring intervention. Treatment is generally started on babies between 5 weeks and 5 months of age. Because of this window of time, it’s important to note any hemangiomas to your baby’s doctor as soon as you notice them.
Hemangeol is administered twice a day, given to your baby right before or right after feeding them. Your doctor will gradually increase the dosage, then readjust dosage regularly as your baby’s weight changes. Treatment generally lasts 6 months, continuing until your baby is 12 months old – though in some cases, it may last longer.
Hemangeol comes with a graduated oral dosing syringe and syringe adapter for easy administration, and comes in strawberry and vanilla flavors to help your baby take their medicine without a fuss.
Treatment Outlook
60% of patients reached a complete or nearly complete resolution of their IH within 6 months. In trial studies, Hemangeol greatly outperformed the placebo, where only 4% of infants saw such promising results. 88% of infants on Hemangeol saw improvement after just 5 weeks of treatment.
Side Effects
Side effects of Hemangeol tend to be mild and well worth the results it offers. In trials, fewer than 2% of patients stopped treatment due to adverse reactions. The most common side effects of Hemangeol are sleep disorders, aggravated respiratory tract infections, diarrhea, and vomiting.
References
1- Léauté-Labreze et al – Infantile Haemangioma –Lancet 2017 Jul 1;390 (10089): 85-94
2. Munden et al – Incidence and demographics of IH – BJD 2014, 170; 907-913
3. Goelz R et al. Incidence and treatment of infantile hemangioma in preterm infants. Arch Dis Child Fetal Neonatal
Ed 2015; 100 F85-91
4. Volc-Platzer et al. – Poster ESPD 2014
reference at the bottom of the page:
5. Darrow D, Greene AK, Mancini AJ, Nopper A J. Diagnosis and Management of Infantile Hemangioma. PEDIATRICS. 2015 Oct;136(4):1060-1104.4
6. Baselga E, Roe E, Coulie J, Munoz Fania Z, Boon LM, McCuaig C et al. Risk Factors for Degree and Type of Sequelae After Involution of Untreated
Hemangiomas of Infancy. JAMA Dermatol. 2016 Nov;152(11):1239-1243.
Important Safety Information for HEMANGEOL
Do not give HEMANGEOL to your child if your child:
- was born prematurely and has not reached the corrected age of 5 weeks
- weighs less than 4 ½ pounds
- is allergic to propranolol or any of the other ingredients in HEMANGEOL
- has asthma or a history of breathing problems
- has a heart problem, slow heart rate (less than 80 heart beats per minute), very low blood pressure
- is at risk for low blood sugar, for example is vomiting or unable to take feedings
- has high blood pressure caused by a tumor on the adrenal gland, called “pheochromocytoma”
Tell your doctor about all of your child’s medical conditions, all of the medicines your child takes, and all of the medicines that you take if you are breastfeeding your child.
HEMANGEOL can cause serious side effects, including:
Low blood sugar (hypoglycemia), especially if your child is not taking feedings, or is vomiting. HEMANGEOL may make it more difficult to recognize the signs and symptoms of low blood sugar in your child. To help reduce the risk of low blood sugar with HEMANGEOL, give HEMANGEOL during or shortly after feeding your child. Feed your child regularly during treatment. Tell your doctor if your child has a poor appetite. If your child is not taking feedings, due to an illness or vomiting, do not give HEMANGEOL until your child is taking feedings normally again.
If your child has any of the signs or symptoms of low blood sugar listed below during treatment with HEMANGEOL, stop giving your child HEMANGEOL and call your doctor or go to the nearest emergency room right away.
Signs or symptoms of low blood sugar include: pale, blue or purple skin color, sweating, irritability, crying for no apparent reason, irregular or fast heartbeat, poor feeding, low body temperature, unusual sleepiness, seizures, breathing stops for short periods of time, and loss of consciousness
If your child is conscious, give him/her a drink of a liquid containing sugar.
Other serious side effects can include:
- New or worsening slow heart rate (bradycardia) or low blood pressure (hypotension).
- Breathing problems or wheezing.
- Stroke. HEMANGEOL may increase the risk of stroke in certain children who have severe problems with the blood vessels in their brain, particularly if your child has a large hemangioma that affects the face or head.
Call your doctor or go to the nearest hospital emergency room if your child has:
- pale skin color, slow or uneven heartbeats, arms or legs feel cold, blue or purple skin color, or fainting.
- breathing problems or wheezing during treatment with HEMANGEOL.
The most common side effects include: sleep problems, worsening respiratory tract infections, diarrhea, and vomiting.
These are not all the possible side effects of HEMANGEOL. Call your doctor for medical advice about side effects.
You are encouraged to report negative side effects of prescription drugs to the FDA. Visit www.fda.gov/medwatch or call 1-800-FDA-1088.
Please see Full Prescribing Information and Medication Guide.